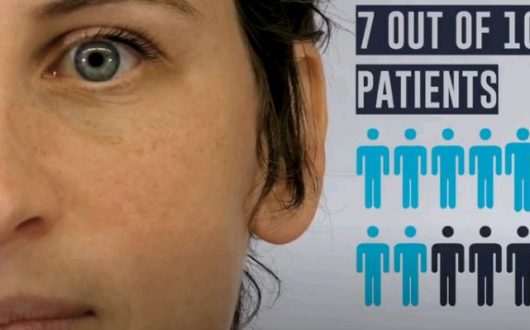
System changes implemented through the BOOST initiative resulted in 7 out of 10 patients retained in therapy.
The number of deaths caused by drug poisoning far exceeds the deaths caused by the COVID-19 pandemic in British Columbia. The BC Coroners Services report states that 1,202 people have died this year from illicit drugs. Many of these fatalities occurred in a private residence when people with an opioid use disorder (OUD) were using at home alone.
Now more than ever, we urgently need community-based harm reduction services and safe supply to support people with opioid dependency.
How healthcare workers are working together to save lives
One group of health professionals tackling the opioid crisis is the Vancouver Best Practices in Oral Opioid Agonist Therapy collaboration (BOOST), which was launched in partnership with the BC Centre for Excellence in HIV/AIDS (BC-CfE) and Vancouver Coastal Health. In 2017, 20 healthcare teams across Vancouver joined forces with a common goal of improving care for clients living with OUD.

BOOST: Provincial Congress brings together healthcare workers across B.C. to solve gaps in the system for people with opioid use disorders.
Through the Vancouver BOOST collaboration healthcare workers are now doing a better job of identifying clients lost to care, and then reconnecting them to community healthcare services that are essential in their recovery.
Tracy Rapanos, Director, Community Services at Coast Mental Health, is a member of the BOOST network. Tracy explains that there are a number of barriers that prevent people from reaching the three-month mark of Opioid Agonist Therapy (OAT), which provides treatments that include Suboxone and methadone to treat opioid dependency, reduce drug-related harms, and support long-term recovery.
“Keeping people on track with their recovery requires a team of nurse practitioners, social workers and mental health workers,” says Rapanos. “When people are going through treatment they still have opioid dependency, so healthcare workers are a vital piece of the puzzle. Healthcare practitioners provide the wraparound daily supports people need to encourage them to take their medications and attend appointments, among other things.”
Rapanos explains that people going through OAT can get overwhelmed and forget to pick up their prescriptions or attend follow-up healthcare appointments. Healthcare workers provide daily check-ins to encourage people to make healthy choices.
“When people relapse it signals a gap in the healthcare system that needs to be fixed,” adds Rapanos. “Many of these gaps can be filled by adding wraparound supports.”
young adult oat pilot program:
As part of the Vancouver BOOST collaboration, Coast Mental Health partnered with the Foundry – Inner City Youth clinic at St. Helen’s Hotel. Together, they co-manage 19 rooms for young adults aged 19-24. Youth living at this facility have experienced severe substance use disorders, mental health concerns and homelessness.
In 2018, there were 24 overdoses by 11 different young adults at this facility, with one overdose resulting in a death. Both Coast Mental Health and the Foundry were interested in understanding how they could better support young adults, of whom accounted for 47 per cent of overdoses at this site.

Left to right – Keren Mitchell, Nurse Practitioner, Foundry, Matt Piercy, Peer Support, Foundry, and Yvonne Paquette, Youth Social Worker, Coast Mental Health, create opportunities to talk about Opioid Agonist Therapy (OAT) with tenants through games and treats.
In early 2019, Coast Mental Health and the Foundry piloted an OAT clinic for young people living at St. Helen’s Hotel. The clinic is offered twice a week and includes outreach services, which requires staff to knock on doors to encourage tenants to take their medications and attend doctor appointments.
Yvonne Paquette, a Coast Mental Health youth social worker at St. Helen’s co-facilitated the pilot OAT clinic with other healthcare practitioners from the Foundry (Vancouver). Together, they found creative ways to engage young adults in conversations about OAT, encouraging 21 young adults to seek support through the in-house clinic. But, as Paquette and her team learned, there were still a number of challenges in supporting people in their recovery.
“Through the pilot OAT clinic, we discovered the healthcare system wasn’t set up to help people with OUD,” says Paquette. Take for instance walk-in health clinics; places the public can access to manage their personal wellness. Unfortunately, these clinics are not set up for people who are going through drug withdrawal and very sick, and in excruciating pain. Just sitting in a clinic waiting for an appointment to see a doctor can be torture for someone with opioid dependency, which makes it less likely they’ll get the treatment they went to the clinic for, let alone return for further treatment.”

One of 21 young adults benefiting from the pilot OAT clinic.
The young adult on-site OAT clinic has only been in operation for 11 months, but already the data indicates improved engagement with clients and less occurrences of overdoses caused by drug poisoning at this site.
“With an in-house clinic and wraparound supports, we’ve seen an average of seven out of 10 people remain in therapy as opposed to three out of 10 people at three months of OAT, say Paquette.”
While the pilot program has now finished, the two-day clinic continues to support youth living at St. Helen’s. The program results have also given the BOOST collaborative a number of valuable insights, but most importantly, the finding suggest that people with opioid dependency need a safe space to access harm reduction supports, treatments and safe supply.
“There’s an urgent need for community-based harm reduction strategies to support people with substance use disorders,” explains Darrell Burnham, CEO, Coast Mental Health. “While many of our sites have harm reduction rooms and resources to support people with substance use disorders, it’s still not enough. We cannot reach everyone with an opioid dependency. In my experience, our best approach is not only providing people with harm reduction services and substitution treatments, but ultimately we need a safe drug supply people can access when they need it.”

As part of Mental Illness Awareness Month and World Mental Health Day last month, Coast Mental Health launched a campaign with the aim of ensuring the government makes funding mental health a key priority.
We have made five recommendations of support focusing on social determinants of health and wellness that influence our mental health. This week, we’re adding our voice to the public debate on harm reduction services and safe supply.
We believe substance use is a health issue and in order to save lives we need to provide people with opioid dependency with harm reduction services to put them on a path to recovery.
Here’s how you can help:
- Read our 5 recommendations
- Use your voice and pledge your support
- Organize your own fundraising events to support our mission
- Donate today to one of our causes
- Volunteer with us
- Partner with us on a solution in mental health